Rheumatoid arthritis or RA is a chronic autoimmune disease that primarily affects the joints, causing inflammation, pain, swelling, and stiffness.
It occurs when the immune system mistakenly attacks the body’s own tissues, particularly the synovium, which lines the joints.
This results in inflammation that can damage cartilage, bone, and other joint structures, leading to joint deformity and loss of function.
RA’s Prevalence Across Ages: What? Why?
- Juvenile Idiopathic Arthritis
In children (16 and below), the common form of arthritis is known as juvenile idiopathic arthritis (JIA).
As of 2021, approximately 3 million children globally are affected by JIA, underscoring the significant impact of this chronic condition on the pediatric population.
Unlike RA in adults, JIA encompasses several subtypes, each with distinct characteristics and prognoses. JIA is also often harder to diagnose partly due to the fact that joint pain is common among children.
Symptoms often include persistent joint pain, swelling, and stiffness, which can significantly impact a child’s growth and physical development. Early diagnosis is crucial, as untreated JIA can lead to severe complications such as joint damage and growth abnormalities. The biggest difference between JIA and RA in adults is that children can often outgrow JIA with the help of treatment.
- RA in adults
Although RA can occur at any age, it is more common to develop in adults 60 years old or younger, which is also labeled as early onset RA by doctors.
This autoimmune disorder leads to chronic inflammation primarily in the joints, causing pain, swelling, and stiffness that can severely impact daily activities and quality of life. Women are more likely to develop RA than men, and hormonal factors may play a role in its onset and progression.
In adults, RA can lead to significant disability if not adequately managed, as prolonged inflammation can cause joint damage and deformities.
- RA in the elderly
RA in the elderly, also known as elderly-onset RA (EORA), presents unique challenges and often differs in presentation compared to younger adults.
Typically diagnosed in individuals over the age of 60, EORA may exhibit more acute onset with prominent systemic symptoms such as fever, fatigue, and weight loss, alongside the characteristic joint pain and stiffness.
Elderly patients often face additional health complications, including comorbidities like cardiovascular disease and osteoporosis, which can complicate RA management.
What Are The Factors Contributing To RA Across All Ages?
Although the true cause of RA is still not known, it is believed that its development is influenced by a combination of genetic, environmental, hormonal, and immune system factors.
- Genetic Predisposition
A family history of RA significantly increases the risk of developing the disease. Specific genetic markers, such as the HLA-DRB1 gene, have been linked to a higher susceptibility to RA, indicating that hereditary factors play a crucial role in the disease’s onset.
- Environmental Factors
Various environmental triggers contribute to the development of RA. Smoking is one of the most well-documented risk factors, especially in genetically predisposed individuals[1]. Infections and exposure to certain bacteria and viruses can also initiate or exacerbate the autoimmune response. Additionally, occupational exposures to silica and other industrial pollutants have been linked to an increased risk of RA.
- Hormonal Influences
Hormonal factors, particularly in women, influence the prevalence and severity of RA. The disease is more common in women, and hormonal changes related to pregnancy, childbirth, and menopause can affect disease activity. Estrogen, in particular, is thought to play a role, although the exact mechanisms are not fully understood.
- Immune System Factors
RA is primarily an autoimmune disorder, where the immune system mistakenly attacks the body’s own tissues. Dysregulation of the immune system, including the overproduction of pro-inflammatory cytokines, leads to chronic inflammation and joint damage. Factors that influence immune system function, such as infections and gut microbiota, can contribute to the onset and progression of RA.
Management And Treatment
While there is no cure for RA, effective management and treatment require a comprehensive approach that includes medications, lifestyle modifications, and, in some cases, surgical interventions.
The cornerstone of RA treatment is medication, which can be categorized into several classes:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs) – These are used to relieve pain and reduce inflammation. Common examples include ibuprofen and naproxen.
- Corticosteroids – Drugs like prednisone can quickly control inflammation and suppress the immune system but are generally used for short periods due to potential side effects.
- Disease-Modifying Antirheumatic Drugs (DMARDs) – These drugs, such as methotrexate, sulfasalazine, and hydroxychloroquine, slow the progression of RA and prevent joint damage by targeting the underlying autoimmune process.
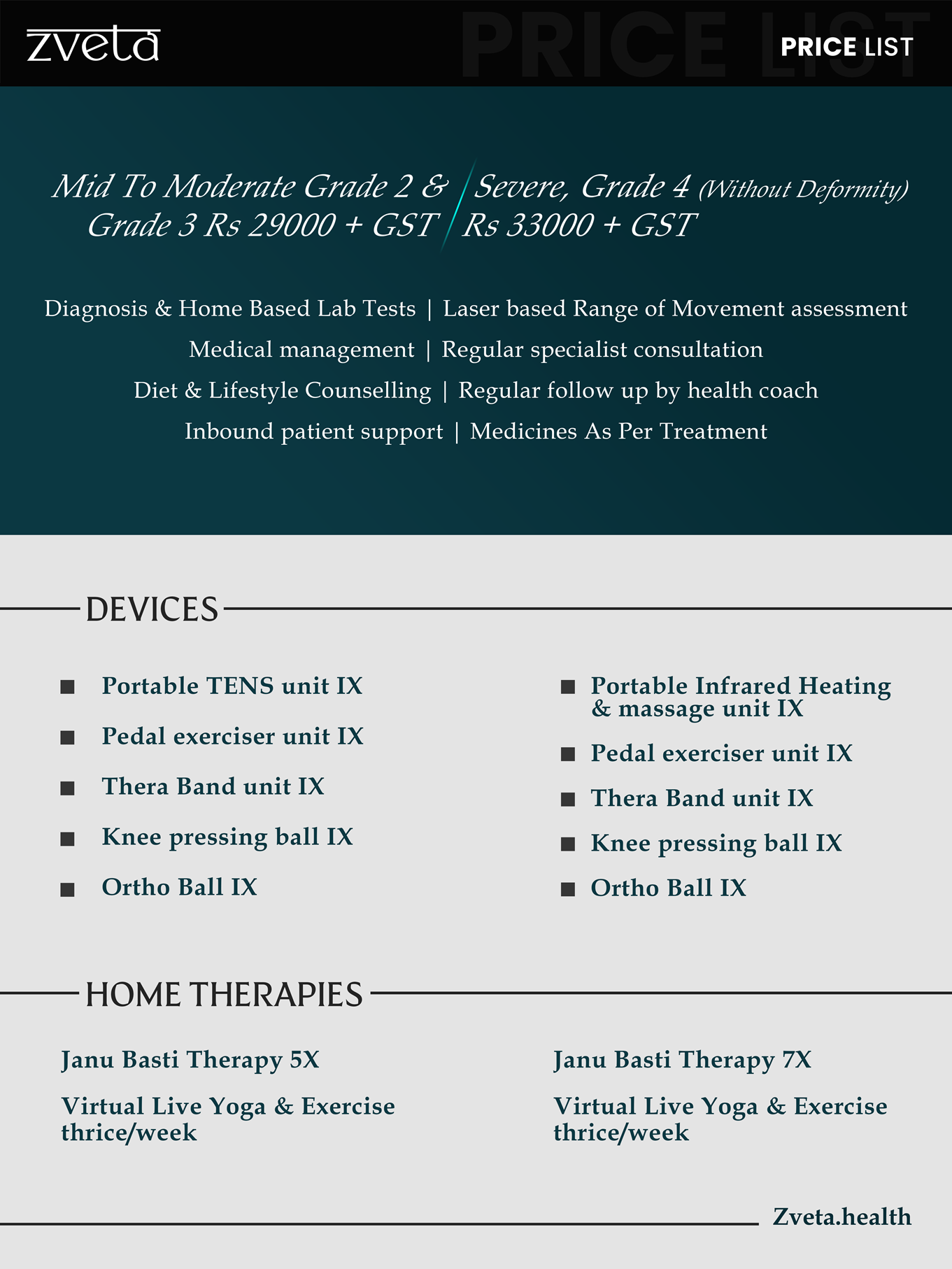
You can also discover the secret to a pain-free life with Zveta Health’s non-invasive, personalized arthritis treatment. Embrace Ayurveda, yoga, and a balanced diet, all from the comfort of your home!
Regular physical activity can help maintain joint flexibility, muscle strength, and overall physical function. Low-impact exercises such as swimming, walking, and yoga are particularly beneficial.
On top of that, a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can help manage inflammation. In cases where joint damage is severe and non-surgical treatments are ineffective, surgery may be considered.
Concluding thoughts
Rheumatoid arthritis (RA) is a complex and challenging disease that can affect individuals of all ages, from children to the elderly. While the true cause of it is still being studied, various genetic and environmental factors might contribute to its onset across the ages.
Early diagnosis and aggressive treatment are important to manage RA effectively and prevent joint damage. Advances in medical treatments, including the development of biologics and targeted therapies, have significantly improved the outlook for those with RA, helping to control symptoms and prevent joint damage. Early and comprehensive management can help individuals with RA lead active and productive lives.